After all, the call center is a doorway that not only represents your digital brand but maybe the first – and only – impression a patient or provider will need to form an opinion. In addition, safety is a significant indicator of the products a consumer will choose.
Broad digital transformation across the healthcare ecosystem means that merely providing a call line is no longer enough. Support needs to be convenient, seamless and offered across multiple channels.
If your call center relies on manual agent processes, disparate systems, a network of direct dial numbers, even small amounts of call volume can lead to a poor patient, provider, agent, and pharmacist experiences. Furthermore, call center managers can’t resolve issues, predict volume, or coach agents because data cannot be quickly aggregated.
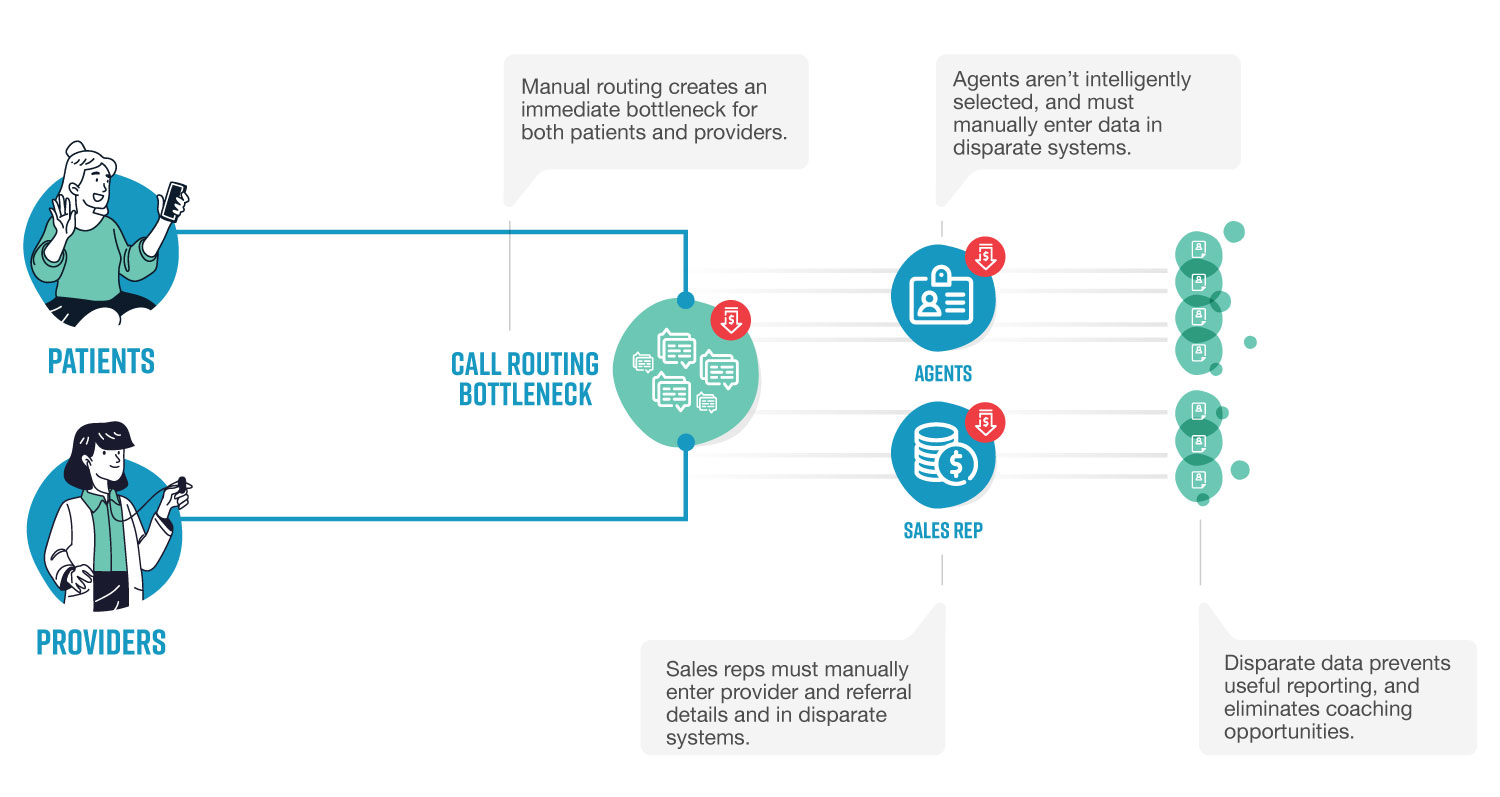
These are the pains at the core of the specialty pharmacy call center…and they have consequences on operational efficiency, employee morale, and revenue.
Bottlenecks, Poor Experiences, and Revenue Loss
Many pharmaceutical companies have tried to assemble an array of disparate systems to solve their call center challenges.
At a high level, every specialty pharmacy support center needs to address the following types of inquiries:
Patient Support
- General questions about product information
- Questions about current prescriptions, side effects, dosage, and more
- Questions about existing orders
Provider Support
- Medical affairs services
- Referral Management
- Sales Support
However, the challenges created by routing bottlenecks, manual data entry, and siloed systems make serving patients and providers difficult.
Patients want answers, and they want them quickly and assertively – after all, your health is in their hands. But, unfortunately, bottlenecks, lack of tech infrastructure, and disparate data lead to the following pains.
Providers need quick information about medications and even faster access to medical affairs info.
Here is an overview of a typical pharmacy’s call center.
The inefficiencies are apparent, and they lead to pain for your key stakeholders – including patients, providers, and internal pharmacy staff.
Patients
- High call volume results in long on-hold times
- Lack of automation makes it difficult to connect patients with the right agent
- Call spikes mean that patients end up in voicemail
Providers
- Can’t solve medical affairs (involving questions about medications, patients) because they have trouble reaching the correct resources
- Can’t submit referrals easily because there isn’t a self-service portal (results in loss of revenue and loyalty for pharmacy)
Additionally, employees in the call center itself have pain:
Internal Staff
Agents
- High call volume leads to agent burnout
- Dealing with patient or provider requests with no insight into how to solve them (lack of a knowledge base, tiered support, etc.)
- Manual data entry (often in decentralized spreadsheets) leads to poor agent performance
- Lack of self-service options for patients means menial questions are asked repeatedly
- Agents don’t have insight into the fulfillment side of the business because they work in a different system
- Unable to solve commonly recurring questions by referencing previous answers
Pharmacists and Nurses
- Have to answer patient phone calls because agents aren’t equipped to answer questions (meaning they can’t focus on their jobs)
- Don’t have insight into aggregate patient concerns because they work in a different system.
Leadership
- Low customer satisfaction scores
- Unable to make data-based decisions to improve service
- Unable to make data-based decisions to lower call times and reduce cost
- Losing referrals due to poor provider referral management
- Losing variable compensation as a result of poor agent performance
Call Center Manager
- Unable to improve call center performance due to technical infrastructure
- Supervisors unable to manage agents due to disparate systems
- Unable to establish clear objectives with senior management because there is no baseline
- Lack of productivity and call metrics to gain insight into call center supervisors and their agents
- Unable to aggregate stats across supervisors to distinguish high-performing teams
- Unable to create long or short-term forecasts for adaptive call coverage
- Unable to proactively track KPIs and change course based on metrics
- Unable to analyze overall performance, especially after adjusting processes intended to boost performance
Wow, that’s quite a list!
In order to find remedies to these pains, we’re going to take individual dives into each stakeholder – patients, providers, and call center staff.
Part 2 is available! Read it here.