What can we help you find?

Case Study
A Platform for Provider Management
See how Penrod automated prior authorizations and streamlined processes with a cloud-based provider management platform built in Salesforce.
Learn More

Our client is a local, nonprofit, managed care organization focused on improving the health of Texas residents. They offer one of the largest portfolios of affordable or no-cost plans that serve one of the largest provider networks.
In order to provide the best member experiences, our client strives to make preauthorization as efficient as possible. In the insurance industry, prior authorization can be a massive bottleneck, taking anywhere from one day to months for care to be approved. Delays in the process may postpone care, cause patients to require an ER visit, and impact a provider's revenue cycle management. This results in negative member and provider experiences.
Our client relied on utilization management (UM) to manually evaluate requests for procedures, tests, and medications. In order to improve member experiences, reduce administrative work, and decrease operational costs, they needed to consider automated solutions.
Manual processes for care authorization increased wait times, reduced operational efficiency, increased cost, and impacted provider relationships
Implementing Salesforce Health Cloud with provider self-service portals to automate prior-authorizations
Faster authorizations, higher member satisfaction, and reduced operational cost
Preauthorization is not easy to automate for a couple of reasons. First, most systems aren't flexible enough to power an end-to-end authorization workflow. They often don't have consistent data models, integrate with clinical systems, or support attachment standards.
Despite this, automation is the best way to fix the problems that manual authorization processes create for members and providers.
Members
Manual preauthorization tactics were not only an administrative burden but a major risk to impact member satisfaction negatively. Any delay in authorization could result in lapsed care, negative healthcare outcomes, or unexpected trips to the emergency room. Any of these factors can create negative member experiences, unexpected bills, and higher overall claim costs.
Additionally, manual utilization management processes not only affected timelines but also raised operational costs.
Providers
Without a self-service portal, it wasn't always clear which procedures, medications, or products would require prior authorization. Additionally, requests were often incomplete or inaccurate because the manual processes - usually sent via phone, email, or fax - didn't set clear requirements for preauthorization requests. As a result, even minor errors - such as incorrect addresses, names, or medical scenarios - could result in a timely back-and-forth process that frustrated the member or provider.
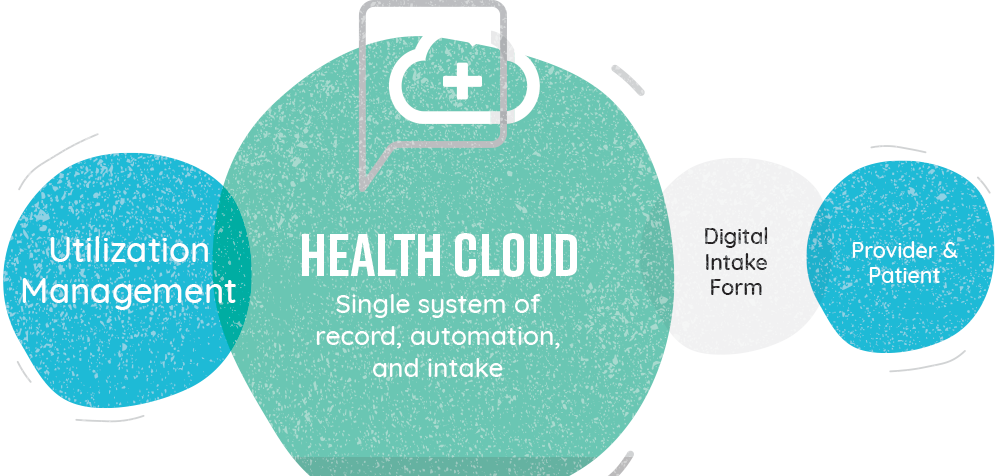
Our client's search for a unified provider management platform that could handle provider self-service and reauthorization automation ended with Salesforce Health Cloud.
Self-service Portals
Health Cloud ensured that clear standards would help providers submit complete, accurate authorization requests the first time. Digital, web-based intake forms offered self-service options to providers, greatly reducing administrative burden by lowering call and fax volume.
Authorization Automation
Authorization requests from the self-service portal were created as cases in Health Cloud, meaning that approvals were tracked, organized, and accessible. In addition, standard workflows automated manual processes, meaning that patients could be connected with their needed care faster than ever before.
As a result of Penrod's Health Cloud implementation, our client saw a number of immediate improvements.
Clear standards and digital forms ensured providers send the right information, the first time
Utilization management staff no longer focused on tactical, administrative tasks
Faster authorization quickly connects patients with the care they need