Solving the Use Case
Overview
There are a variety of requirements needed to solve the credentialing use case with Salesforce. At the highest level, credentialing platforms need to:
- Allow physicians to apply through digital applications
- Create declarative workflows with automations, trigger alerts, and task assignment
- Integrate with with authorities like CAQH, NPPES NPI, Sam.gov, and major EHRs
Additionally, we generally configure two basic permission sets in Salesforce to achieve this use case. They are:
- Credentialing
- Contracting
Now, let's run through how we solve each requirement in Salesforce.
Meeting the Requirements
Digital Applications
Penrod utilizes a third-party form component for gathering CAQH data and other pre-employment specifics crucial for jumpstarting the credentialing process. One of our top HIPAA-compliant form tools is Titan, known for its remarkably user-friendly form creation process, empowering us to link fields to any object or field within Salesforce.
Field mapping plays a pivotal role in ensuring data accessibility throughout the credentialing journey, typically encompassing details related to a provider's background, licenses, and education. With the exchange of sensitive information like social security numbers, email addresses, names, and physical addresses, the entire process is secured with a digital certificate for TLS/SSL encryption over an HTTP protocol. Other information we collect could include:
- Gender
- Ethnicity
- Phone Number
- Resume
- Licenses
- Board Certifications
- NPI Number
- Qualifications
Clearly, forms can get complicated. The time-to-revenue clock starts when a provider begins filling out the application. Faster form completion means faster credentialing. As a result, it's important to implement time saving features that remove road blocks to prompt completion. Penrod expedites form submission by customizing URLs to auto-fill data from primary sourced data, like CAQH. We also prevent providers from losing progress and enabling them to pick up where they left off later on.

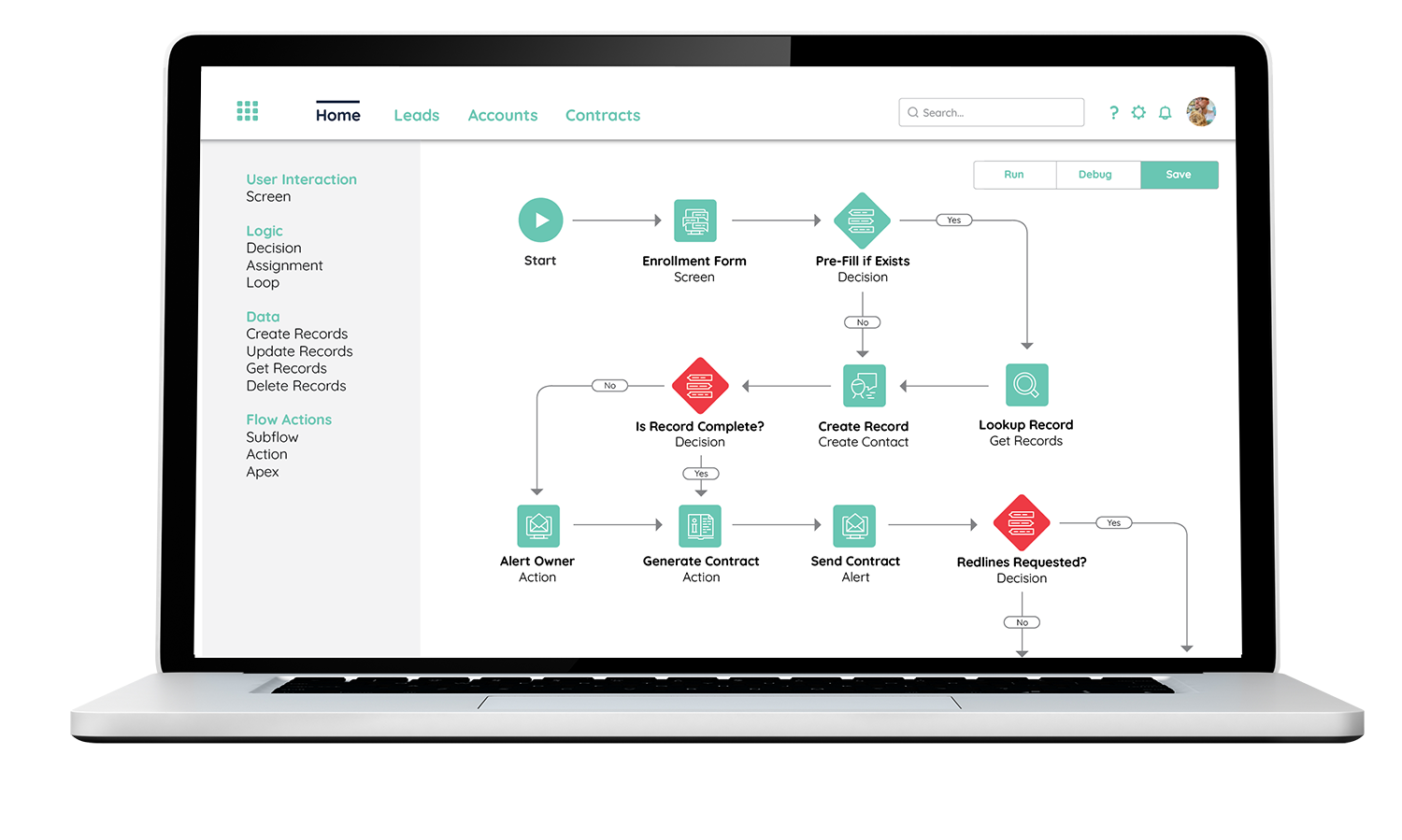
Declarative Workflows
Declarative workflows kick in right after an application is sent. When we talk about declarative workflows, we're referring to processes tailored to a specific use case. This setup allows us the freedom to execute automations, set off alerts, and tweak processes in real-time.
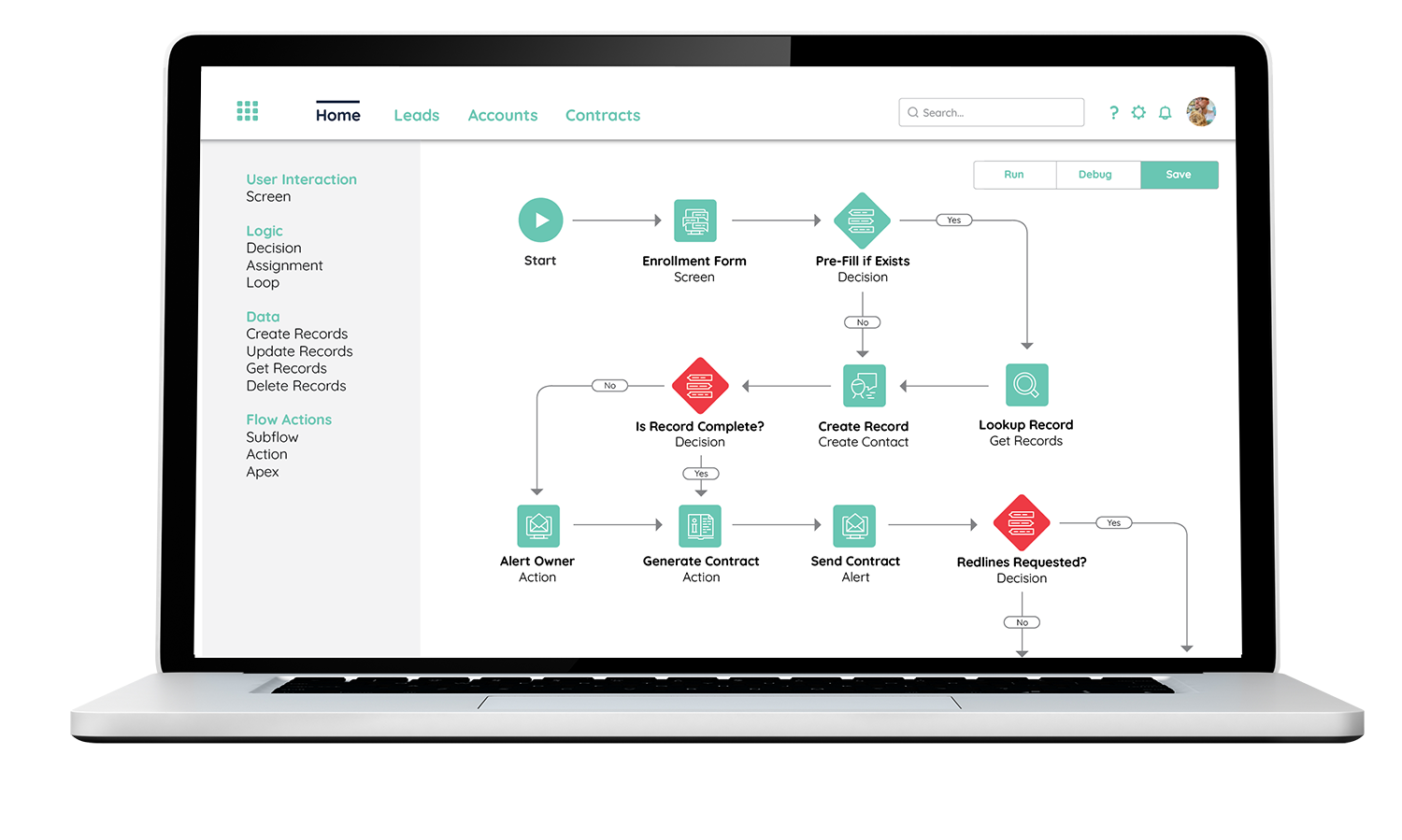
This is where Salesforce excels, and why its customization makes it an ideal platform for the credentialing use case. We activate Salesforce workflows at various points during the credentialing process. Through the lightning interface, these points can trigger specific layouts, user alerts, tasks, and more to expedite the process. So, once an application is submitted, an applicant is generated under the lead object. This object houses all the necessary info a medical staff manager needs to evaluate applicants, validate their credentials, and kickstart contracting without manual data entry. The high level lightning flow includes stages for application submitted, verification, contracting, and credentialed.

Unified Data
The entire credentialing process involves accessing multiple data sources for verification. Manually checking each one leads to significant delays in the process. By consolidating them within the Salesforce interface under one dashboard, we offer an instantaneous view to the care manager specialist or whoever is verifying an application.
Here are some common data sources Penrod integrates into the care manager dashboard to solve this use case:
- SAM.gov
Verify provider eligibility for receiving federal funds like Medicare
- ABMS Board
Ensure providers meet national education and experience standards through continuous learning
- Checkr and Clearcheck
Confirm provider background checks
- CMS Preclusion Lists
Identify providers unable to accept Medicare Advantage
- OIG LEIE
Identify providers excluded from federal healthcare programs
- Deanumber
Identify retired or suspended pharmaceutical licenses
By uniting all these sources into a single credentialing platform, staff no longer need to switch between multiple sources to verify providers.
![]()