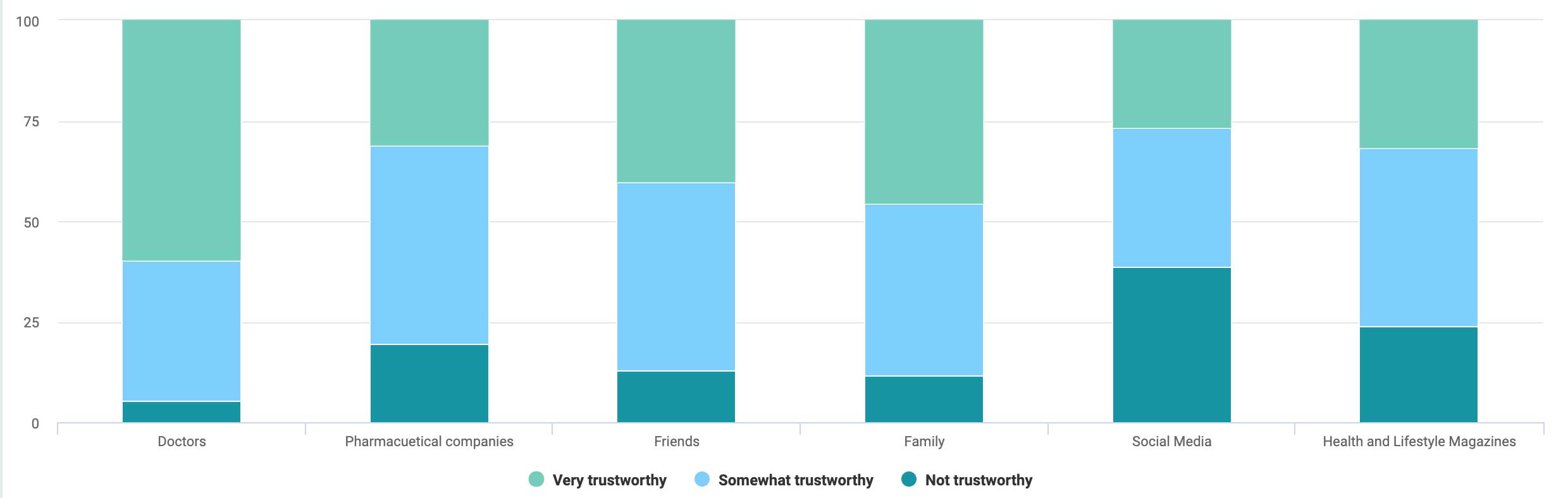
A recent Penrod research survey found that the majority of consumers we asked trusted doctors most for advice about prescriptions. Pharmaceutical companies themselves ranked 2nd to last, narrowly beating social media.
This highlights the importance of building strong relationships with providers and physicians. Doctors are your most important advocate for introducing patients to your medications, and you need to support them in innovative ways.
In order to build the most successful referral network, it’s important to address the pain providers face when submitting referrals, seeking medical affairs service, or looking for product information. Providing a better provider experience than your competitors will attract more providers, generate more referrals, and produce more revenue.
A virtual call center is a unified platform that provides your sales agents, medical staff, and technicians with access to the data, insights, and knowledge bases they need to handle questions about products, requests for referrals, and consultations about patients.
Let’s look at a few specific provider pains that virtual call centers solve.
Key Pains
Pain: Lengthy Referral Cycles
Every provider knows that a lengthy referral cycle creates negative patient experiences. Lengthy referral cycles not only reflect poorly on your pharmacy but, also providers. Negative experiences bubble up from the patient to the provider, and then to you.
Referral times can be drastically reduced with a provider relationship management platform. These platforms help specialty pharmacies by empowering broader physician networks to sell their medications more efficiently.
This includes automated intake of incoming physician referrals, activity tracking across multiple channels, and automated alerts that keep referrals moving as quickly as possible. As a result, there is complete visibility into every referral, regardless of source.
Pain: Paper-Based Referrals
Paper-based referrals transfer accountability to the patient. Not only are they slower than electronic referral solutions, but they also pose a risk to revenue leakage – after all, there is no guarantee that the patient will actually fill the prescription. As a result, adding paper-based inefficiencies to the patient’s responsibilities leads to procrastination, anxiety, and poorer healthcare outcomes.
Paper-based referrals can be replaced by digital intake portals. This allows a physician to easily place a referral by filling out a secure, HIPAA-compliant form that instantly sends the referral to your pharmacy. As a result of the tight integration between the form and your pharmacy management platform, the referral is instantly received, categorized, assigned – and then tracked throughout the full referral lifecycle.
Pain: Consultation Experience
In order to provide compliant, effective consultation support, pharmacies can no longer rely on phone, email, or fax. Not only could these communication methods be non-compliant with HIPAA, but they also cause referrals to take much longer than necessary.
Outdated channels of communication are being replaced by digital consultation portals that allow pharmacies and providers to securely message, exchange patient medical information, and view referral status. This enables real-time insights, transparency, and accountable relationships that eliminate inefficiency in the referral process.
Pain: Poor Medical Affairs Support
Like patients, it’s not uncommon for providers to be transferred from one agent to another. Providers need rapid answers, and any lapse in support results in worse patient outcomes and lower provider satisfaction.
Intelligent call routing is one way this pain point can be resolved. Routing makes call management more efficient. The routing system identifies the caller’s phone number, their reason for calling, and assigns them to the agent – or if needed, immediately escalates to a medical care professional – that can best assist them.
Furthermore, the agent is given a 360-degree view of the provider, their patients, and other details directly in the platform.
Routing systems also help by identifying an agents’ history, skills, and training to ensure the provider is routed to the optimal agent or care staff. If appropriate, the system ensures calls are routed to call-center agents rather than nurses or pharmacists, allowing medical staff to focus on their job responsibilities.
Final Thoughts
Upgrading your call center to a unified virtual support platform can resolve many of your providers’ pain points. By incorporating a knowledge base, syncing your CRM with the call center, and creating a multichannel platform, you will enhance the provider experience, drive more referrals, and increase revenue. Your agents will also benefit from a more automated approach that simplifies crucial, repetitive, and time-consuming tasks. This leaves them with more time to focus on personalized provider service and faster referrals.

